The Indiana Network for Patient Care (INPC) has evolved over the years from a clinical and claims data repository supporting individual patient care into a statewide engine for advancing population health. Titus K. Schleyer, D.M.D., M.B.A., Ph.D., who leads the Learning Health Informatics Program at the Regenstrief Institute in Indianapolis, recently spoke with Healthcare Innovation about a research paper published in BMC Medical Informatics and Decision Making that puts a spotlight on health information exchange in Indiana.
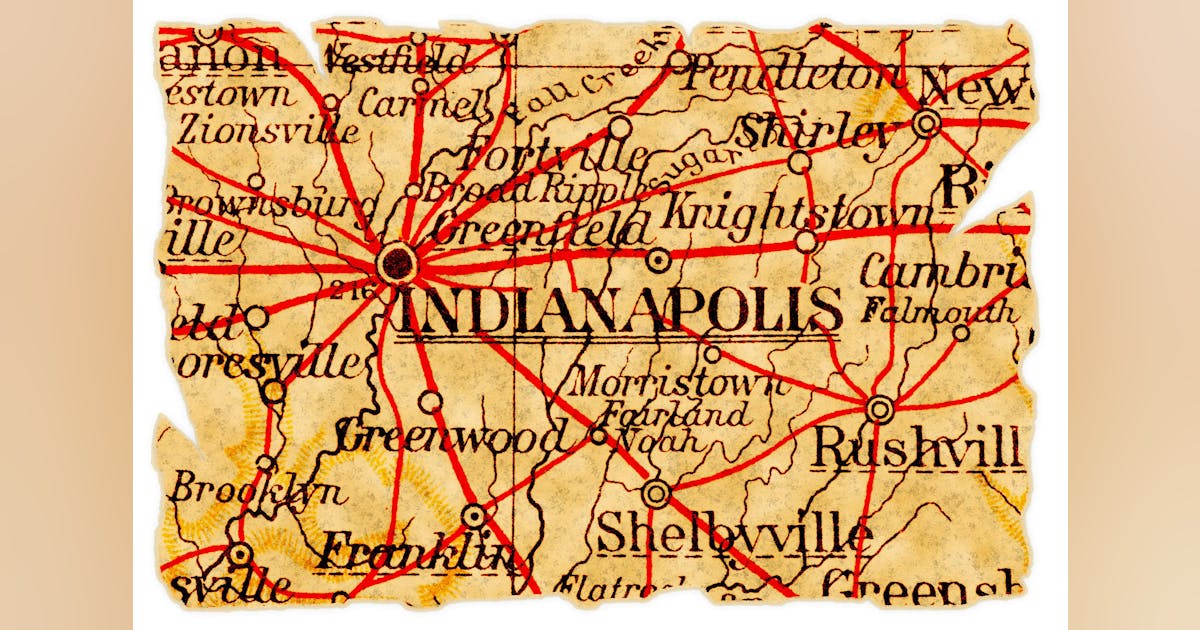
As the researchers note, by the end of its first decade in 2004, the INPC captured data for 3.5 million patients from just nine Indiana counties. But by the end of 2023, it incorporated records for more than 20 million patients, more than 16 billion clinical data elements, and contributions from 123 hospitals, 19,000 practices and 54,500 providers spanning Indiana and spillover regions in southern Michigan, Illinois, Ohio and Kentucky.
Healthcare Innovation: The paper you co-authored makes the case that the building blocks of data sources that INPC put together have laid the groundwork for more sophisticated applications. Is the approach that INPC took different from other health information exchanges — or did they follow a similar approach to CRISP in Maryland or other successful HIEs?
Schleyer: Even though most health information exchanges started at different places, they all have to eventually end up making these building blocks. So I wouldn’t say we figured it out and nobody else did.
HCI: But were there some things unique to its formation, or the provider landscape in Indiana that made the INPC a little more robust than HIEs in other states, or was the involvement of Regenstrief impactful?
Schleyer: Regenstrief was very successful early on in attracting a diverse group of healthcare providers into the health information exchange. And as some health systems grew into statewide entities, such as IU Health, we got geographic coverage pretty quickly, and we also attracted labs and physician practices and other places. So I think that probably makes the INPC a little bit qualitatively different from many of the others.
HCI: Did Regenstrief provide some of the informatics tools to help transform the health records into meaningful insights?
Schleyer: Yes. The INPC was spun off from Regenstrief into a separate not-for-profit entity called Indiana Health Information Exchange (IHIE) around 20 years ago. Before then, Regenstrief wrote all the tools to make the HIE work. It got into analytics. HIEs were built for clinicians to exchange data about their patients, right? Only later did we recognize that this is a big, valuable resource upon which we can build analytics and insights. So that came later. In 2004 IHIE licensed most, if not all, software that Regenstrief had written to build the health information exchange, and then IHIE started to develop its own things, and Regenstrief kept doing analytics on the data resource. To this day, we have a carbon copy of the live INPC on Regenstrief computers, and people like me do analytics on that data set.
HCI: The paper mentioned an Indiana Addiction Data Commons. Could you describe what that is and who’s involved?
Schleyer: The addiction crisis is a generalized problem for lots of places. The question is, how do we identify people who have substance use disorder? How do we identify people at risk of going to the emergency room for an overdose? The Indiana Addictions Data Commons was built as a special-purpose data collection that facilitates research around this public health problem, and it came out of the Indiana Addiction Grand Challenge, which is now over. It was a five-year project funded by IU, but the data resource is still there.
HCI: Are there still challenges around sharing behavioral health data and substance use data as part of the IHIE?
Schleyer: It’s a very good question, and the answer is yes. If you want to get a really good handle around substance abuse, you can’t just look at health data. You have to look at things like justice involvement. To know if this person had encounters with the police or the justice system that touched on addictions or substance use disorder, you need ambulance data. The EMS systems know who overdosed, but that information typically does not make it into the INPC, right? One of the big challenges for managing addictions and substance use disorder is bringing the data together. Right now we have this mosaic where lots of pieces are missing, and we’re looking at the mosaic and asking what kind of picture is this? Well, if we had more pieces to the mosaic, we’d actually be able to recognize the picture much better.
HCI: One of the things the paper mentions is that the INPC data is critical for Indiana’s accountable care organizations. Could you talk about ways in which those ACOs rely on this data?
Schleyer: An ACO can do better the more complete data it has about its patients. Patients don’t always go to the same healthcare provider. They sometimes go down the street instead of back to that mother healthcare system. For quality measure reporting, ACOs need the most complete data that they can get about each of their covered lives. So if the measurement is HbA1c monitoring, if I only have my data as a healthcare system, I might miss some of the HbA1c tests the patient has had, and if I’m below the threshold, I don’t get as much money for that patient. But if I get the data from other health systems where they had their HbA1c checked and integrate that in my data, It better reflects the full care they’re getting.
HCI: I spoke to you two years ago about Health Dart, a FHIR-based clinical decision support tool that integrates information from the HIE directly into the EHR. At the time, it was running in 15 emergency departments at IU Health. Have there been some developments since then?
Schleyer: The product is essentially the same. The EDs use it, but IHIE is working quite hard to get it into the Epic App Store so that more local health systems can use it off the shelf. That’ll make it much easier to get it out to other health systems, especially those who run Epic.
HCI: In writing this paper, are there some lessons learned from INPC that other HIEs could put in place?
Schleyer: One of the things that I would position very high as a lesson for other HIEs is to try to build a similar trust relationship that we have between healthcare institutions and IHIE.
The more we invest in a common resource, and we have a common vision about what this thing does and how it benefits everybody who invests and contributes to it, the more benefit we get out of it. It is completely the opposite of what you see in many places today.
HCI: Hospitals and health systems in a lot of these big cities say we’re on Epic, and all the other big hospitals here are on Epic. They use Care Everywhere, so they say it’s not worth their effort to invest in health information exchange. But the fact is that there are lots of providers who aren’t on Epic and that share data from small offices, from behavioral health providers or FQHCs and the health systems are not getting that data.
Schleyer: That is correct. Epic has done a really good job with their products and the infrastructure. There’s no question that they’ve had a transformative effect on healthcare. But as you just said, they don’t cover everything, and the case that our paper makes is that in order to help people become and stay healthy, you really need to know a lot of different things. You mentioned behavioral health. You mentioned FQHCs, long-term care facilities. You know, the integration of medical records between long-term care facilities and health systems is terrible. Regenstrief has a big research effort in that area, too.
Will Epic rule the world at some point and have software in all different things? Well, maybe that’ll happen, but it’s not now, so we need to be a little bit more cognizant of the fact that we need to make efforts to to integrate more different data that are not in Epic systems.
I also get it from a healthcare system perspective. The margins are tight. They always worry about costs and revenue. We don’t have a compelling equation that says, If you link all the data together, your healthcare costs would sink by 30%. If we had that, it would be wonderful. But the fact is, we can do better for patients and populations if we understand more what their health is, what their context is.
One of the things I’m working on is now is the intersection of sustainability and climate change and health informatics. We’re talking about who is at risk during heat waves and who’s likely to die during a heat wave. We need to know who are the people who have no access to cooling, who are the people who are taking medications that don’t work as well when there’s a heat wave. That way, we could do much better keeping at people safe from harm, but we don’t have these systems yet in a very mature fashion that help us do that. So that’s another use case for HIE — helping build resilience in the face of more and more severe consequences of climate change.
link