Database and data collection
This retrospective cohort study used data from the Korea Disease Control and Prevention Agency COVID-19 National Health Insurance Service cohort, which is linked to the Korea Disease Control and Prevention Agency and the National Health Insurance Service. The Korea Disease Control and Prevention Agency data provided general characteristics such as sex, age, date of diagnosis of confirmed COVID-19 patients, and COVID-19 vaccine data, and the National Health Insurance Service provided claims data, including patient information (age, sex, primary diagnosis, admission date, discharge date, etc.) and hospital information (number of beds, number of nurses, region, etc.). Data on confirmed COVID-19 cases from October 8, 2020, to October 29, 2022, can be linked with National Health Insurance Service data. In this study, data were extracted based on patients who had been hospitalized among patients who could be linked to the National Health Insurance Service with confirmed COVID-19 data. Based on this, a total of 1,387,345 patients were included in the baseline.
Inclusion criteria for this study were patients admitted to a medical institution with a diagnosis other than COVID-19. There were 591,155 hospitalized patients at baseline, of which 253,451 were diagnosed with COVID-19 based on the International Classification of Diseases codes (U071 and U072) during hospitalization or had COVID-19 onset dates confirmed before and after hospitalization in data from the Korea Disease Control and Prevention Agency. Patients diagnosed with COVID-19 were those who tested positive by a polymerase chain reaction or rapid test in a healthcare facility. The exclusion criteria considered the characteristics of both the medical institutions and individuals. First, we excluded medical institutions that had less than 30 beds, did not submit nurse staffing levels and thus could not confirm the nurse-to-patient (bed) ratio, and did not have nurses. According to the Medical Act, in Korea, inpatients are admitted to hospitals or general hospitals. Hospitals must have 30 or more beds, and general hospitals must have 100 or more beds, operate at least seven specialized departments, and have specialists. Among general hospitals, those that provide difficult procedures to patients with severe conditions are designated as tertiary hospitals. This study included only patients admitted to hospitals, general hospitals, and tertiary hospitals. Second, patients aged under 18 years, aged over 80 years, with no income level, or with a length of stay of 0 days were excluded. This study included only adult patients, so only adult ICUs were included, thus excluding pediatric or neonatal ICUs. In addition, since the comprehensive nursing service wards are operated under a system different from that of the general ward, only patients admitted to the general ward were included; finally, patients admitted with the primary diagnosis of COVID-19 were excluded. To consider potential HA COVID-19 as suggested in previous studies18, patients who were not diagnosed with COVID-19 during hospitalization but were confirmed to have COVID-19 within seven days after discharge were also included. Further, because there is a possibility of HA COVID-19 owing to factors other than nurses during long-term hospitalization39, patients whose hospitalization periods exceeded 31 days were excluded. Ultimately, 1376 hospitals and 61,267 patients were included in this study.
Variables
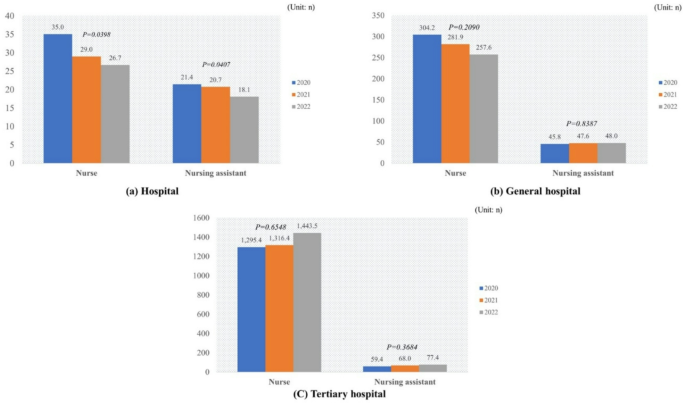
The variable of interest in this study was nurse staffing. Nurse staffing levels were measured based on claim data, and ICUs were classified into nine nurse staffing levels based on the nurse-to-bed ratio, while general wards were classified into seven nurse staffing levels based on the nurse-to-patient ratio. This study classified each of these levels into five categories for ICUs (nurse-to-bed ratio: < 1:0.5, < 1:0.77, < 1:1.1, < 1:1.5, and ≥ 1:1.5) and general wards (nurse-to-patient ratio: < 1:2.0, < 1:3.0, < 1:4.5, < 1:6.0, and ≥ 1:6.0). The fixed night-shift nurse system is part of the flexible work system, where fixed-shift night nurses work eight hours a night, up to 14 days a month, and each nurse must handle no more than 25 patients. This policy was applied to hospitals excluding Seoul in April 2017, expanded to hospitals and general hospitals excluding Seoul in October 2019, and expanded to tertiary hospitals including Seoul from January 2022. The National Health Insurance Service provides incentives to medical institutions based on the proportion of fixed night-shift nurses among all nurses (< 10%, < 15%, < 20%, < 25%, ≥ 25%). In this study, institutions were classified into six categories, including institutions that do not operate fixed night-shift nurses. Additionally, the proportion of nursing assistants among all nurses was classified based on quartiles (< 5%, < 15%, < 30%, and ≥ 30%).
The outcome variable was HA COVID-19 infection during hospitalization. HA COVID-19 was defined as a person diagnosed with COVID-19 within seven days after hospitalization or confirmed with COVID-19 within seven days after discharge, referring to existing nosocomial infection definitions and previous studies18. Hospital characteristics included type of hospital (hospital, general hospital, and tertiary hospital), region (capital area, metropolitan, and other), and number of beds (< 300, < 500, < 700, < 900, and ≥ 900). Patient characteristics included sex (female and male), major diagnosis (respiratory system [International Classification of Diseases codes: J00–J99], malignant neoplasm [International Classification of Diseases codes C00–C97], circulatory system [International Classification of Diseases codes I00–I99], and other), age (≤ 40, ≤ 55, ≤ 65, ≤ 75, and > 75 years), Charlson comorbidity index, health insurance (employee, self-insured, and Medicaid), income (low, low-moderate, moderate-high, and high), and year of admission (2020, 2021, and 2022). In addition, to consider patients’ movements, we evaluated whether the hospital and the patient’s residence were in the same location. We also considered the number of doses of COVID-19 vaccine before hospitalization. Finally, because infection rates can also potentially impact HAIs, we included the COVID-19 incidence rate per 1,000 population by region by month.
Statistical analysis
The distribution of each categorical variable was examined by analyzing frequencies and percentages, and χ2 tests were performed to examine HA COVID-19. Either a t-test or ANOVA was performed to compare the average values and standard deviations for continuous variables. Survival analysis using the Cox proportional hazards model was used to analyze the association between HA COVID-19 and nurse staffing, adjusting for other covariates. In addition, to evaluate differences according to the timing of COVID-19 infection, HA COVID-19 was evaluated during hospitalization (seven days after hospitalization) and after discharge (within seven days after discharge). All statistical analyses were performed using SAS (version 9.4; SAS Institute).
link